Pain is one of the body’s most common warning signals, and millions of people around the world rely on painkillers (analgesics) every day to ease discomfort from headaches, injuries, arthritis, or chronic conditions. Whether purchased over the counter or prescribed by a doctor, painkillers play a vital role in healthcare. But how exactly do they work, and what are the benefits and risks of using them? This guide explains the science behind how painkillers work, the key types of pain relief medication, and practical tips on safe usage.
What Are Painkillers?

Painkillers, or analgesics, are medications designed to reduce or block pain signals in the body. Unlike anesthesia, which induces numbness or unconsciousness, analgesics specifically target pathways in the nervous system or inflammatory response without shutting down overall awareness. Broadly, they are divided into two categories:
- Non-opioid painkillers (e.g., paracetamol/acetaminophen, NSAIDs like ibuprofen, aspirin).
- Opioid painkillers (e.g., morphine, oxycodone, fentanyl).
Some other medications, such as certain antidepressants, anticonvulsants, and local anesthetics, can also be used for specific pain conditions.
Main Types of Painkillers and How They Work
1. Paracetamol (Acetaminophen)
- Mechanism of Action: Works mainly in the central nervous system (CNS) by reducing the production of prostaglandins, chemicals that amplify pain signals. Unlike NSAIDs, it does not reduce inflammation in the tissues Mayo Clinic.
- Benefits: Generally safe, effective for mild-to-moderate pain (headaches, muscle aches, back pain).
- Risks/Side Effects: Overdose can cause severe liver damage, especially when combined with alcohol.
2. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Common examples: ibuprofen, naproxen, aspirin, diclofenac.
- Mechanism of Action: NSAIDs block enzymes called COX (cyclooxygenase), which produce prostaglandins responsible for pain, fever, and inflammation. Some, like COX-2 inhibitors, are designed to target inflammation with fewer stomach side effects Cleveland Clinic.
- Benefits: Reduce pain, fever, and swelling (useful for arthritis, menstrual cramps, injuries).
- Risks/Side Effects: Long-term use can increase the risk of stomach ulcers, bleeding, kidney damage, and heart problems Mayo Clinic.
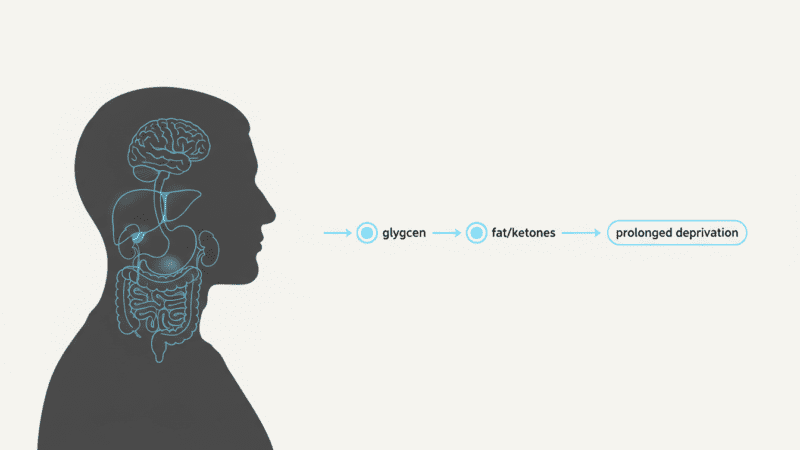
3. Opioids
Examples: morphine, oxycodone, codeine, fentanyl.
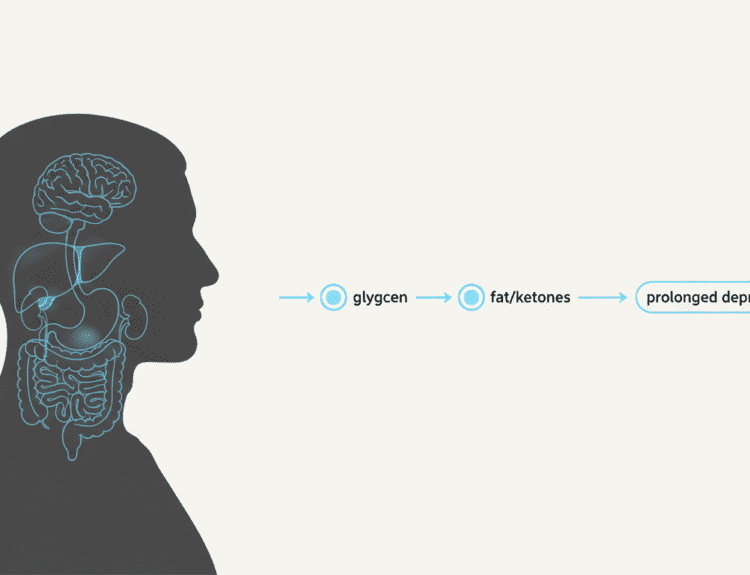
- Mechanism of Action: Bind to opioid receptors in the brain, spinal cord, and gut. They block pain messages and mimic the body’s natural endorphins, creating strong pain relief NCBI StatPearls.
- Benefits: Highly effective for severe pain (cancer, surgery, significant injury).
- Risks/Side Effects: Can cause drowsiness, constipation, nausea, and at higher doses, respiratory depression. Long-term usage poses risks of tolerance, dependence, and addiction Mayo Clinic.
4. Other Pain-Relieving Medications
- Antidepressants (e.g., amitriptyline, duloxetine): Enhance serotonin/noradrenaline activity to reduce chronic nerve pain StatPearls.
- Anticonvulsants (e.g., gabapentin, pregabalin): Calm overactive nerve firing in conditions like neuropathy or fibromyalgia.
- Local anesthetics (e.g., lidocaine patches): Block sodium channels in nerves to prevent pain signals from transmitting.
Benefits of Painkillers
- Improve quality of life by reducing pain intensity.
- Allow recovery from injuries, surgeries, and chronic illnesses.
- Over-the-counter (OTC) options are widely available for short-term relief.
Risks and Side Effects
- Overuse or misuse can cause organ damage (liver, kidneys, heart).
- Opioids carry a strong risk of tolerance, dependence, and overdose.
- NSAIDs may cause stomach bleeding and cardiovascular issues.
- Mixing painkillers with alcohol or other drugs increases risks.
Safe Usage Guidelines
- Follow recommended dosages exactly.
- Do not mix multiple painkillers (e.g., NSAIDs with aspirin) without medical advice.
- Limit alcohol use to reduce liver and stomach damage.
- Use the lowest effective dose for the shortest necessary period Cleveland Clinic.
When to Consult a Doctor
Seek medical advice if you:
- Need painkillers daily for more than a few days.
- Experience stomach bleeding, jaundice, or unusual side effects.
- Have chronic conditions like kidney, liver, or heart disease.
- Suspect tolerance or dependence on opioids.
Conclusion
Understanding how painkillers work in the body helps patients make safer, informed choices when managing pain. From everyday remedies like paracetamol to prescription opioids for severe conditions, each type interacts with the body’s nervous system and inflammatory pathways differently. While these medicines can be powerful allies, they must be used responsibly. When in doubt, consult a healthcare professional before starting or combining pain relief medications.